A Shot in the Arm Can Prevent Cervical Cancer

KARACHI, Jul 26 (IPS) - “Listen to your body, and if there is anything strange happening, do not ignore it,” is the advice of 57-year-old Afshan Bhurgri, a cancer survivor.
Eight years ago, she was diagnosed with cervical cancer at a time when she was “in a good place” in life. Her kids were grown up, and she had more time to herself. A fitness freak, the schoolteacher’s daily routine included going to the gym daily. “I joined a creative writing class as I loved penning my thoughts!” she reminisced.
But then everything changed when she found out she had cancer.
Cancer of the cervix uteri is the fourth most common cancer among women worldwide, with an estimated 604,127 new cases and causing the death of 341,831 in 2020.
In Pakistan, an estimated 73.8 million women over the age of 15 are at risk of developing cervical cancer caused by the human papillomavirus (HPV).
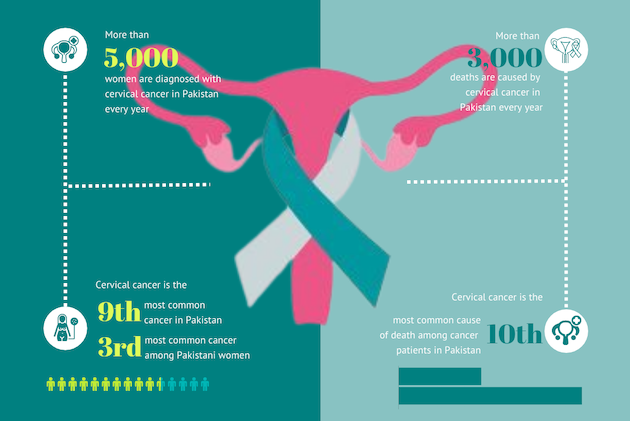
In the absence of complete data, it is estimated that of the 5,000 women diagnosed with this cancer in Pakistan, some 3,000 lose their lives every year due to lack of access to prevention, screening and treatment, thus making it the third leading cause of cancer-related deaths in women of the reproductive age group in the country, after breast and ovarian cancers. Up to 88 percent of cervical cancer cases are due to human papillomavirus (HPV) serotypes 16 and 18, as reported by the International Agency for Research on Cancer.
“We are short on authentic data on the prevalence of the disease burden,” said Dr Arshad Chandio, who works at Jhpiego Pakistan as an immunisation lead. His organisation, which has supported HPV vaccine introduction in seven countries with Gavi support, is partnering with the federal and provincial governments, along with WHO, UNICEF, and USAID, to implement a roadmap for cervical cancer prevention and introduction of HPV vaccine in Pakistan. Cervical cancer is the only cancer that is preventable by a vaccine.
“Without authentic data, our plan to eradicate this disease will not be watertight,” admitted Dr Irshad Memon, the director general of the Expanded Programme on Immunisation in Sindh.
Dr Shahid Pervez, senior consultant histopathologist at the Aga Khan University Hospital (AKUH), co-chair of the country’s newly established National Cancer Registry, recommends legislation to make reporting of cancer mandatory. “This will be one way of collecting basic data, at one place, which is expected by international agencies to roll out an effective cancer control programme in Pakistan,” he added.
Although Bhurgri had knowledge about cancer of the cervix and went for regular health checkups and screenings, her doctors did not carry out full examinations, which led to the infection turning cancerous. It all started in 2009, five years prior to being diagnosed with cancer when she started noticing a “foul smell emanating from my vagina” after her period became “heavier” than usual.
“Let alone screening and testing for the cancer, many healthcare professionals do not even know of the disease, or how women get infected,” pointed out Chandio.
“I am an educated person, I could afford to get the best medical help, and I went to three of the city’s top gynaecologists, got pap smears done on their requests over the years, and I was only sent for HPV test when it was too late,” rued Bhurgri. In 2014, a doctor suggested an ultrasound which gave a true picture. A biopsy confirmed she had cervical cancer.
After her biopsy, Bhurgri started reading up on cervical cancer, and one of the indications was the foul vaginal smell.
“It could have been nipped in the bud if only the doctors had carried out a thorough examination,” said gynaecologist and obstetrician Dr Azra Ahsan, president of the Association for Mothers and Newborns, blaming “sheer negligence” on the part of her fraternity.
“A gynaecological consultation must not only be limited to a conversation across the table,” said Ahsan, but should include an “examination on the couch including a proper internal examination, ideally a pap smear and visual inspection,” especially if, like Bhurgri, a patient was complaining of heavy bleeding and a foul smell.
Bhurgri’s journey towards wellness was tough. A radical hysterectomy was recommended, and her cervix, her uterus and her ovaries were removed. Twenty-eight radiations and five chemos later, over a five-month period, she was given a clean chit by her oncologist. The cost of treatment, back in 2014 at a private hospital, was a whopping Rs30,000,000 (USD 1,097) back then.
Screening can save lives
Although Bhurgri’s cancer may have remained under the radar despite regular screening via pap smears, doctors say HPV and pap smear tests are the best way to screen a woman for cervical cancer. They can identify patients who are at high risk of developing pre-cancerous changes on the cervix as well as pick up those who have already developed these changes.
These precancerous lesions can be treated before they turn into cancer. Sadly, in Pakistan, the uptake of pap smears is negligible and estimated to be as low as 2 percent.
According to Dr Uzma Chishti, assistant professor and consultant gynecologic oncologist, Department of Obstetrics and Gynecology, AKUH, Pakistan’s health system is so financially stretched that it cannot afford to provide screening of women by these expensive tests. Instead, she recommends WHO’s recommendations of performing a visual inspection of the cervix by acetic acid (VIA) to screen women to help reduce the incidence of cervical cancer. “VIA is an alternative screening test for low-and-middle-income countries like ours,” she said.
Vaccinations the Best Option
The WHO triple intervention recommendation to eliminate cervical cancer in countries like Pakistan includes scaling up HPV vaccination to 90 percent for girls aged between 9 to 14, twice-lifetime cervical screening to 70 percent and treatment of pre-invasive lesions and invasive cancer to 90 percent by 2030. “All three are essential if we want to eliminate cervical cancer completely,” emphasised said Ahsan.
HPV vaccinations to prevent cervical cancer are the way forward as it provides primary prevention, said Chishti, in the absence of VIA, screenings and pap smear tests. Almost 60 per cent of cervical cancer cases occur in countries that have not yet introduced HPV vaccination. Pakistan is one of them.
Once up and about, the first thing Bhurgri did was get her 14-year-old daughter vaccinated for human papillomavirus (HPV) vaccine. “My older daughter remains unvaccinated as she was 21 then and studying abroad. She needed three shots and could not make it to that timeline,” she said.
In Pakistan, two globally licensed HPV vaccines are available in the market - a quadrivalent vaccine and a bivalent vaccine Cervarix. Gardasil is protective against the HPV serotypes 6, 11, 16, and 18, providing protection against both cervical cancer and genital warts. Cervarix is effective against serotypes 16 and 18, thereby protecting only against cervical cancer.
In 2021, medical students at the AKUH interviewed 384 women attending outpatient clinics between the ages of 15 to 50 to find out their knowledge about cervical cancer. They found that of the 61.2 percent of women who had heard about cervical cancer, 47.0 percent knew about pap smear tests, and among them, 73 percent had gotten a pap test. A total of 25.5 percent of women, out of the 61.2 percent, knew that a vaccine existed for prevention, but only 9.8 percent had been vaccinated against human papillomavirus. The study concluded that a majority of the women interviewed for the study belonged to a higher socioeconomic class and were mostly educated, yet their knowledge regarding the prevention and screening of cervical cancer was poor. “This reflects that the knowledge levels as a whole would be considerably lower in the city’s general population,” the study concluded.
Shamsi highlighted the challenges of discussing HPV in a conservative society where sexual health topics are hardly discussed due to the embarrassment and taboo associated with sexually transmitted infections (STIs). This communication conundrum has resulted in a general lack of information about the disease. “There is a total lack of information about HPV, cervical cancer, and its prevention among the masses,” she said.
But this may change if Pakistan introduces the HPV vaccine at a national level, utilising routine effective and established immunisation delivery strategies. According to Dr Uzma Shamsi, a cancer epidemiologist at the AKUH, implementing the HPV vaccine at a national level in Pakistan could save hundreds of thousands of lives annually.
The benefits are enormous, and hundreds of thousands of lives could be saved each year, she emphasised.
Pakistan is in talks with Gavi the vaccine alliance, to support the country in including the single-dose HPV (two covers four strains) vaccine in its routine immunisation programme. “It will probably take another two years and USD 16 million before we can roll out the vaccine, but when it happens, it will be a country-wide campaign,” confirmed Memon.
Shamsi predicted some tribulation because the primary target group for vaccination is pre-adolescent girls. “A new vaccine for a new target age group comes with its own set of challenges in a society where conspiracy theories about vaccination programmes, stigma and misinformation about cancer and sexual health persist,” she said. And so before the actual rollout, Shamsi emphasised, it was important to increase awareness about the HPV virus, cervical cancer causes, and vaccine’s safety and usage among the general public, patients, and healthcare professionals while actively dispelling misinformation.
Memon agreed that “conversation around the vaccine must begin”. For its part, the Sindh government set aside Rs 100 million ($365,884) for advocacy of HPV vaccine uptake in its current budget. “We will initiate a dissemination campaign once we know when the HPV vaccination programme is to begin,” he said. The Sindh province was also the first to initiate the typhoid conjugate virus vaccine after an extensively drug-resistant virus was found in the province. He was hopeful there would be less resistance to the HPV vaccine after the successful administration of measles and rubella and the pediatric Covid-19 vaccines earlier.
However, said Memon, “We will need more women vaccinators this time as young girls are shy of rolling their shirt sleeves up for male vaccinators.” With up to 125,000 female health workers across Pakistan, who were earlier trained by Gavi for MR immunisation, which is a much more difficult vaccine to administer (being subcutaneous) as opposed to the HPV one (which is muscular), he said, this workforce can be engaged to get trained for this vaccination campaign too.
In the end, however, according to Chandio, “without a strong political will and leadership, a national HPV vaccination programme cannot become a reality in Pakistan to eliminate this largely preventable cancer among women”.
Fighting her cancer has changed Bhurgri in more ways than one. Her message to women is to “not put yourself aside; make yourself a priority.” While she continues to lead a healthy life – going to the gym, eating healthy, resting, she said, “You cannot go on and pick up where you left off”.
IPS UN Bureau Report
Follow @IPSNewsUNBureau
Follow IPS News UN Bureau on Instagram
© Inter Press Service (2023) — All Rights Reserved. Original source: Inter Press Service
Where next?
Browse related news topics:
Read the latest news stories:
- Trapped by Tradition: The Widows of Ukerewe and the Ritual They Cannot Escape Friday, April 04, 2025
- Myanmar quake: Airstrikes continue despite ceasefire Friday, April 04, 2025
- Energy Transfers Lawsuit Against Greenpeace Is an Attempt to Drain Our Resources and Silence Dissent Friday, April 04, 2025
- Global Disability Summit Galvanizes Education Support for Crisis-Impacted Children with Disabilities Thursday, April 03, 2025
- World Autism Awareness Day 2025: Sustainable Development Must Include Neurodivergent Perspectives Thursday, April 03, 2025
- Solar-Powered Spinning Machines Help Indian Women Save Time and Earn More Thursday, April 03, 2025
- DR Congo: Millions Facing Destitution as Violence Forces People to Flee Multiple Times Thursday, April 03, 2025
- ‘Every piece tells a story’: Bombs to beauty, from Gaza to Ukraine Thursday, April 03, 2025
- DR Congo: Armed violence displaces thousands as cholera outbreak worsens Thursday, April 03, 2025
- World News in Brief: Israeli military escalation in Syria, Nicaragua rights probe, South Sudan talks Thursday, April 03, 2025