Superbugs Among Top 10 Threats to Whole Cycle of Life
MADRID, Apr 11 (IPS) - Research after research, world's scientists renew their loud alerts against the high dangers of human-driven “superbugs” - bacteria and pathogens that no longer respond to antimicrobials, making infections harder to treat and increasing the risk of disease spread, severe illness and death.
No way.
The pressure of giant industrial sectors appear to be heavier than the needed political well to reduce the dangerous impacts of the excessive use of those drugs which are widely employed to prevent and treat infections in humans, aquaculture, livestock, and crop production.
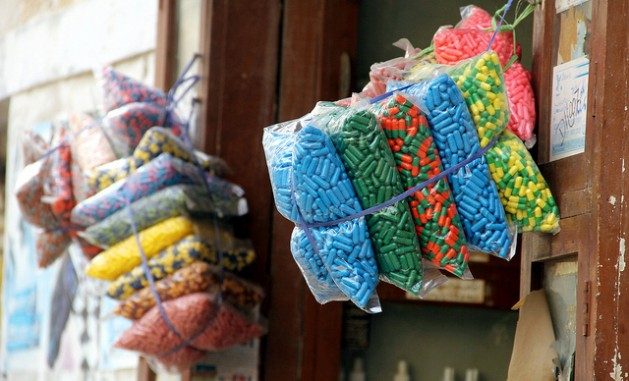
Antibiotics are perhaps the most familiar ones, but there are many others, including numerous antivirals, antifungals and antiparasitic agents that have been largely used and misused to treat diseases but that end up spreading them.
They are known as “superbugs” resulting from their increasing resistance to those medicines. And they are antimicrobial resistant germs which are found in people, animals, food, plants and the environment (in water, soil and air).
“They can spread from person to person or between people and animals, including from food of animal origin,” as further explained by the UN Food and Agriculture Organization (FAO).
Such an increasing abuse of antimicrobials and other microbial stressors (e.g. the presence of heavy metals and other pollutants) creates favourable conditions for microorganisms to develop resistance.
The big threat
They represent one of the most complex threats to global health, and food safety and security. Much so that the World Health Organization (WHO) lists Antimicrobial Resistance (AMR) among the top 10 threats for global health.
The emergence and spread of drug-resistant pathogens that have acquired new resistance mechanisms, leading to antimicrobial resistance, continues to threaten the ability to treat common infections, WHO explains.
Alarming advance of multi-resistant bacterias
“Especially alarming” is the rapid global spread of multi- and pan-resistant bacterias that cause infections that are not treatable with existing antimicrobial medicines such as antibiotics.
“The clinical pipeline of new antimicrobials is dry.” In 2019 WHO identified 32 antibiotics in clinical development that address its list of priority pathogens, of which only six were classified as innovative.
Moreover, estimates suggest that by 2050 up to 10 million additional direct deaths could occur annually. That is on par with the 2020 rate of global deaths from cancer.
Additionally, in the next decade, AMR could result in a Gross Domestic Product (GDP) shortfall of at least 3.4 trillion US dollars annually and push 24 million more people into extreme poverty.
Antibiotics, increasingly ineffective
According to the World Health Organization, the lack of access to quality antimicrobials remains a major issue. Antibiotic shortages are affecting countries of all levels of development and especially in health-care systems.
“Antibiotics are becoming increasingly ineffective as drug-resistance spreads globally leading to more difficult to treat infections and death.”
New antibiotics urgently needed
New antibacterials are urgently needed – for example, to treat carbapenem-resistant gram-negative bacterial infections as identified in the WHO priority pathogen list.
“However, if people do not change the way antibiotics are used now, these new antibiotics will suffer the same fate as the current ones and become ineffective.”
Meanwhile, FAO reports, “the situation is expected to worsen as global demand for food increases,” adding that it is therefore paramount that the agrifood systems are progressively transformed to reduce the need for antimicrobials.
What drives antimicrobials?
As mentioned above, such a threat is primarily driven by the excessive application of antimicrobials, the international body adds. In fact, currently, more than 70% of antimicrobials sold worldwide are used in animals for human consumption.
While AMR occurs naturally over time, usually through genetic changes, FAO reports that their main drivers include:
- misuse and overuse of antimicrobials in human health and agriculture
- lack of access to clean water, sanitation and hygiene for both humans and animals
- poor infection and disease prevention and control in healthcare facilities and farms
- poor access to quality, affordable medicines, vaccines and diagnostics, and
- weak enforcement of legislation.
Who influences the spread of superbugs?
According to UN reports, three economic sector value chains profoundly influence AMR's development and spread:
- Pharmaceuticals and other chemicals manufacturing
- Agriculture and food including terrestrial animal production, aquaculture, food crops or those providing inputs such as feed, textiles, ornamental plants, biofuels, and other agricultural commodities.
- Healthcare delivery in hospitals, medical facilities, community healthcare facilities and in pharmacies where a range of chemicals and disinfectants are used.
Other major consequences
Another leading specialised body, the UN Environment Programme (UNEP) warned in its February 2023 report: Bracing for Superbugs about the need to curtail pollution created by the pharmaceuticals, agricultural and healthcare sectors.
The study focuses on the environmental dimensions of AMR, reporting that the pharmaceutical, agricultural and healthcare sectors are key drivers of AMR development and spread in the environment, together with pollutants from poor sanitation, sewage and municipal waste systems.
Inger Andersen, the UNEP Executive Director, explained that the triple planetary crisis - climate change, pollution and biodiversity loss – has contributed to this.
“Pollution of air, soil, and waterways undermines the human right to a clean and healthy environment. The same drivers that cause environmental degradation are worsening the antimicrobial resistance problem. The impacts of antimicrobial resistance could destroy our health and food systems,” she warned.
Climate, biodiversity, pollution, nature loss…
According to UNEP, global attention to AMR has mainly focused on human health and agriculture sectors, but there is growing evidence that the environment plays a key role in the development, transmission and spread of AMR and is a key part of the solution to tackle AMR.
In fact, AMR is closely linked to the triple planetary crisis of climate change, biodiversity and nature loss, and pollution and waste, driven by human activity, unsustainable consumption and production patterns.
The world leading environmental body explains the following:
- Climate crisis and AMR are two of the greatest and most complex threats the world currently faces. Both have been worsened by, and can be mitigated by, human action.
- Higher temperatures can be associated with increases in AMR infections, and extreme weather patterns can contribute to the emergence and spread of AMR.
- Antimicrobial impacts on microbial biodiversity may affect the cycles of carbon and methane, which are directly involved in regulating Earth's climate.
- Biodiversity loss: Land-use changes and climate change alter soils' microbial diversity in recent decades, and microbes inhabiting natural environments are sources of pharmaceutical discovery.
- Municipal solid waste landfills and open dumps are prone to wildlife and feral animal interaction and can contribute to the spread of AMR.
- Pollution: Biological and chemical pollution sources contribute to AMR development, transmission, and spread.
© Inter Press Service (2023) — All Rights Reserved. Original source: Inter Press Service
 Global Issues
Global Issues